Stories from the University of Cambridge
Autohaem
-
Samuel McDermott[1], Pietro Cicuta[1], Catherine Mkindi[2], Richard Bowman[3]
1 Department of Physics, University of Cambridge, Cambridge, UK 2 Ifakara Health Institute, Bagamoyo, Tanzania 3 Department of Physics, University of Bath, Bath, UK
-
2022
-
McDermott S, Kim J, Leledaki AA, Parry D, Lee L, Kabla A, Mkindi C, Bowman R, Cicuta P. 2022. autohaem: 3D printed devices for automated preparation of blood smears. Rev Sci Instrum 93, 014104.
-
Samuel McDermott:
sjm263@cam.ac.ukPietro Cicuta:
pc245@cam.ac.uk -
https://autohaem.org
-
Cambridge-Africa ALBORADA Research Funding (UK), Global Challenges Research Funding QR (UK) ,Royal Society (UK)
ABOUT THE OPEN-RESOURCE
Background
Blood smears are used for investigating a variety of haematological disorders and parasitic infections. The procedure consists of placing a drop of blood on a microscope glass slide and spreading it using a second microscope glass slide. The thin film of blood is then fixed, stained, and examined on an optical microscope. In large-scale blood testing centres, blood smearing is automated. However, this process is still frequently performed manually in many locations, which is a repetitive and time-consuming task. Samuel McDermott, a post-doctoral research associate in the Biological Physics group, at the Department of Physics, was working on how to automate the diagnosis of malaria using the OpenFlexure microscope (an open source optical microscope, additional information on https://openflexure.org/), when he realised that a lot of the slides sent to him from rural clinics in Tanzania were low quality. “It’s a very hard technique to do manually. And so, I did a bit of research and spoke to some people in some other countries and they were all having the same problem with the manually prepared slides,” says Samuel. He decided to take a step back and improve the blood-smearing stage before focusing on the automation of malaria diagnosis.
Function
autohaem are devices for automated blood smear preparation.
Development process
The devices are composed essentially of two parts: 3D printed ones and electronic components. The 3D parts were designed in a very easy way to print, and there is no need to use a particularly special 3D printer. The electronics can easily be purchased from electronic suppliers. Samuel managed to design a lot of prototypes quickly and then started working on improving them. “It was a very iterative process. In particular, we were looking at two main parameters, which were the speed and the angle that the device uses, and so we did a lot of experiments testing the different angles and speeds and compared it to human experts in the technique. We wanted to be as good as someone who does it every day.” At the moment, Samuel is working with a team of manufacturers in Ethiopia and they have been going through the components to find alternatives that are available in their context.
Target user
Research laboratories especially in low-income countries, where it is more difficult to access equipment. But also, in research labs globally,
as blood smear is usually done by hand.
Comparison to other technologies
Most commercial automated smearing devices on the market are expensive, and use single-use plastic blades as a spreader, generating a lot of plastic waste. The only open design, low cost devices available at the moment are autohaem. Samuel said that as his research goal was to study malaria, they would have used another available tool to make high quality blood smears. However, as there was not anything available, they decided to design it themselves.
IMPACT
Current use
As autohaem are still in the prototype stage, currently they have only been used in the Biological Physics group at the University of Cambridge, and by their collaborators in Tanzania.
Open source choice
“I think the whole purpose of the project would be completely moot if it wasn’t open source, because there’s nothing that the community would gain if it was closed source,” said Samuel. He emphasises how important the idea is of the community for open source development, as speaking to other people who have developed research tools as open source, plus the feedback from the community, helped him to speed up the learning process. However, after being in touch with users in Ethiopia, he is trying to identify what kind of business model will be the best to make the device available for who really needs it. Samuel points out that the open source model works well in Europe, America, and Asia, but that it does not seem to translate very well to lower- and middle-income countries where there is a huge barrier in terms of finding some of the components needed to build the device. “I would love for autohaem to be open source and always kept like that, but also we want to make sure that we can support local manufacturers to be able to make it and sell it in their communities as well. So, some bits of it would have to be commercialised, but it wouldn’t be to make a profit, it would be a social enterprise.”
GOING FORWARD - WHERE TO IN THE NEXT 3-5 YEARS?
Field trials are starting soon in Ethiopia, allowing the device to be tested by a range of users. Once Samuel has completed the field trials, the next step is to start to look for other sources of funding, to be able to turn autohaem into a commercialisable product especially in low- and middle-income countries. The long-term goal is to have the devices used for clinical purposes. However, Samuel is aware that this step will be more difficult to achieve, as the regulatory hurdles for the medical device manufacturing industry in some countries are a big step to overcome.
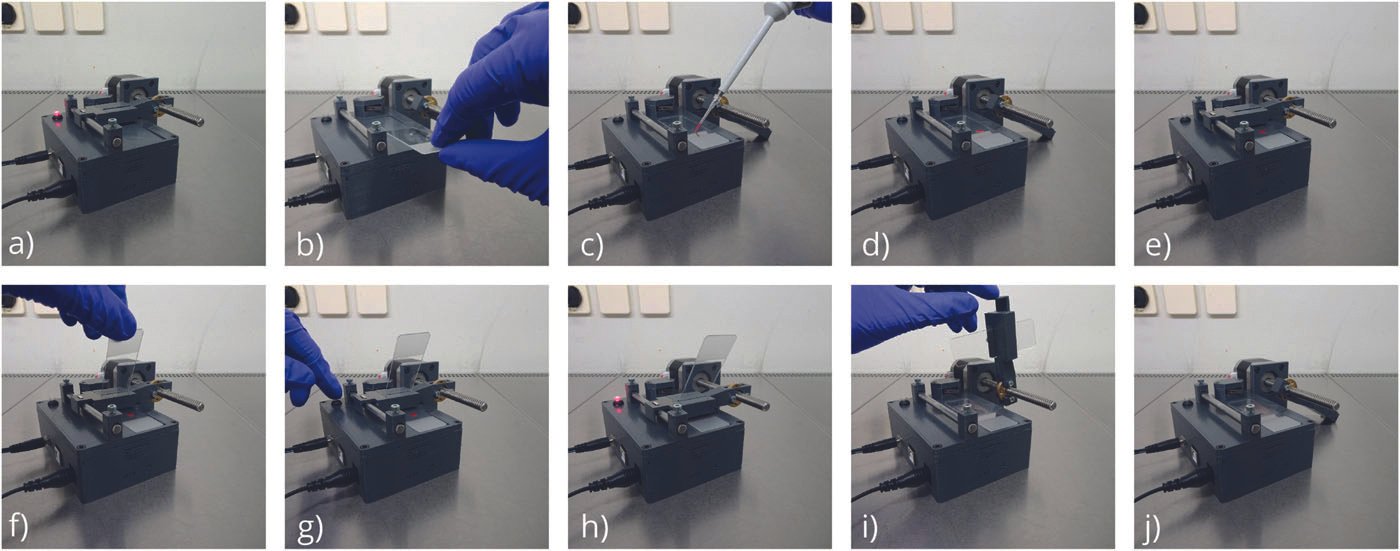
Operation of autohaem smear+. The key steps in the operation of the electro-mechanical device are: (a) plugging in the device; (b) rotating the slider and placing the microscope slide in the slot; (c, d) placing a drop of blood on the microscope slide; (e) rotating the slider into position; (f) inserting the spreader microscope slide; (g) pressing the button to start the smear; (h) device is producing the smear; (i) removing the spreader slide. © 2022, McDermott et al., licensed under CC-BY 4.0. Reproduced from Rev. Sci. Instrum. 93, 014104, https://doi.org/10.1063/5.0076901.
autohaem logo. © 2022, Samuel McDermott, licensed under CC-BY 4.0.